Utilidad clínica de la lámpara de Wood en el diagnóstico de dermatosis inflamatorias, infecciones cutáneas y neoplasias malignas de la piel
2025-05-28 15:20: Fluorescencia amarillo-verde
Tiña de la cabeza (Microsporum spp.):Tono azul verdosoTiña (Trichophyton schoenleinii)
: Señal azul pálido
Tricomicosis axilar
: Luminiscencia blanco-amarilla
Mayoría
Tricófito
las especies lo hacen
no
fluorescencia
Figura 4.
(A) Eritrasma en la región inguinal.
(B) Fluorescencia de color rojo coral observada bajo el examen con lámpara de Wood.
(C) Eritrasma entre los dedos del pie izquierdo, que muestra fluorescencia de color rojo coral bajo la lámpara de Wood.
Infecciones por pseudomonas
Pseudomonas aeruginosa
Emite fluoresceína, detectable como un brillo verde intenso bajo luz ultravioleta. La luz ultravioleta (WL) resulta eficaz para identificar infecciones de heridas y el síndrome de la uña verde, lo que permite un tratamiento antimicrobiano inmediato.
| Figura 5. | (A) Síndrome de la uña verde causado por | Pseudomonas aeruginosa |
|---|---|---|
| . | (B) Madriguera de sarna debajo de la lámpara de Wood (indicada por una flecha blanca). | (C) Imagen dermatoscópica de una madriguera de sarna (indicada por una flecha blanca). |
| Uso en dermatosis parasitarias | Sarna | |
| El examen de WL ilumina las madrigueras de los ácaros como trazos lineales de color blanco azulado, y el propio cuerpo del ácaro a veces brilla de color blanco o verde. La dermatoscopia UV365 mejora aún más la visibilidad de los ácaros, lo que facilita el diagnóstico en casos atípicos. | Aplicación en Oncología y Cirugía Cutánea | Lentigo maligno |
| Delimitar los márgenes de la LM es un desafío debido a la extensión subclínica. Si bien las guías actuales sugieren márgenes quirúrgicos de 5 a 10 mm, un amplio estudio de cohorte indicó que podrían requerirse 15 mm para una tasa de escisión completa del 97 %. | Figura 6. | |
| (A) Nevo lentiginoso maligno en el lóbulo de la oreja derecha, con márgenes clínicos mal definidos. | (B) Delimitación mejorada de los márgenes bajo la lámpara de Wood, lo que permite una identificación precisa de los límites durante la primera etapa de la cirugía micrográfica de Mohs. La flecha negra indica el sitio de una biopsia previa, claramente visible bajo la lámpara de Wood. | |
| Figura 7. | (A) Carcinoma de células basales con márgenes indistintos en el pliegue nasofacial izquierdo. | (B) Demarcación del margen preoperatorio utilizando la lámpara de Wood. |
| (C) Cicatriz postoperatoria tras la escisión de un melanoma en el antebrazo derecho, con extensión clínicamente no aparente antes de la re-escisión planificada. | (D) La lámpara de Wood resalta fácilmente la cicatriz (indicada por la flecha negra). | |
| La lámpara de Wood acentúa los márgenes tumorales ricos en melanina contra la piel normal fluorescente circundante. Su uso preoperatorio en la cirugía de Mohs mejora la evaluación de los límites y puede reducir la recurrencia. Un estudio prospectivo demostró que el mapeo de márgenes guiado por luz blanca se alineó con los márgenes histológicos finales en el 88 % de los casos al añadir un tampón de 5 mm más allá del borde clínicamente visible. | White or yellow luminescence | |
| Pseudomonas Infection | Bright green fluorescence | |
| Microsporum spp. | Green-blue fluorescence | |
| Trichophyton schoenleinii | Pale blue fluorescence | |
| Parasitic | Scabies | Bluish-white tunnels; greenish mite bodies |
| Neoplastic | Lentigo Maligna / Melanoma | Enhanced margin contrast under UV |
| BCC / SCC treated with ALA | Red porphyrin fluorescence | |
| Metabolic | Congenital Erythropoietic Porphyria | Pink fluorescence in body fluids and teeth |
| Porphyria Cutanea Tarda | Pink fluorescence in urine and stool | |
| Hepatoerythropoietic Porphyria | Similar to congenital erythropoietic form | |
| Erythropoietic Protoporphyria | Fluorescence predominantly in blood |
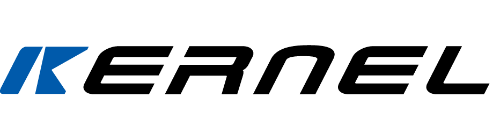
When examined under a Wood’s lamp, lesions of porokeratosis display a characteristic “diamond necklace” pattern — white fluorescent hyperkeratotic scales encircling a central blue-black core (Figure 1A and B). However, this fluorescence is transient and may not be consistently observed.
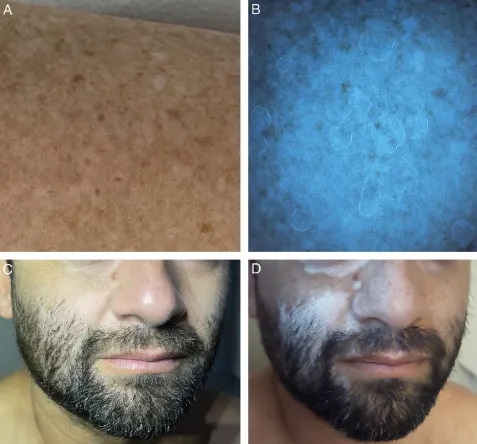
Figure 1. (A) Disseminated actinic porokeratosis. (B) Wood’s lamp examination showing the “diamond necklace” sign, with hyperkeratotic scales exhibiting white fluorescence. (C) Early-stage facial vitiligo. (D) Under Wood’s lamp illumination, the visibility of the depigmented area is markedly enhanced.
Porokeratosis
Wood’s lamp reveals a distinctive “necklace” fluorescence pattern: white margins with darkened central plaques. The fluorescent rim corresponds to the cornoid lamella—this presentation is diagnostically valuable, though transient.
Morphea and Hair Follicle Disorders
In follicular variants of porokeratosis, WL highlights follicular keratin plugs as punctate white signals. In early or subclinical morphea, WL may reveal dark, sharply demarcated patches not visible under ambient light, aiding early therapeutic intervention and longitudinal monitoring.
Applications in Pigmentation Disorders
WL excels in evaluating melanocyte-related anomalies. In vitiligo, the lack of melanin permits deeper tissue fluorescence, yielding a sharply defined blue-white glow. WL is also capable of detecting early or subclinical depigmented macules and quantifying treatment responses. Under UV365 dermoscopy, 40% of lesions reveal uniform fluorescence around hair follicles.
In tuberous sclerosis, small hypopigmented macules (“confetti lesions”) become more prominent under WL, often outperforming visual detection of the classic “ash-leaf” macules.
Melasma
WL assists in assessing melanin distribution depth:
Epidermal: Contrast is heightened under WL
Dermal: No contrast enhancement observed
Histopathological correlation remains variable; some reports affirm WL’s diagnostic value, while others dispute its ability to discriminate between dermal and epidermal melanin accurately.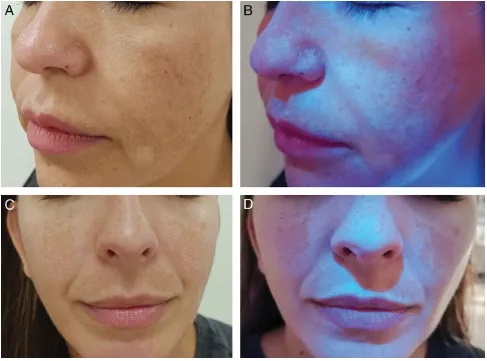
Progressive macular hypomelanosis is a pigmentary disorder caused by Cutibacterium acnes, a Gram-positive bacterium residing in hair follicles that produces coproporphyrin III. Under Wood’s lamp examination, the hypopigmented areas become more distinct, with red fluorescence observed within the follicles in the affected regions (Figure 3A and B). This diagnostic feature aids in distinguishing the condition from others such as tinea versicolor (yellow-green fluorescence), pityriasis alba (non-fluorescent due to irregular parakeratosis), post-inflammatory hypopigmentation, and idiopathic guttate hypomelanosis (blue-white fluorescence indicating dermal involvement).
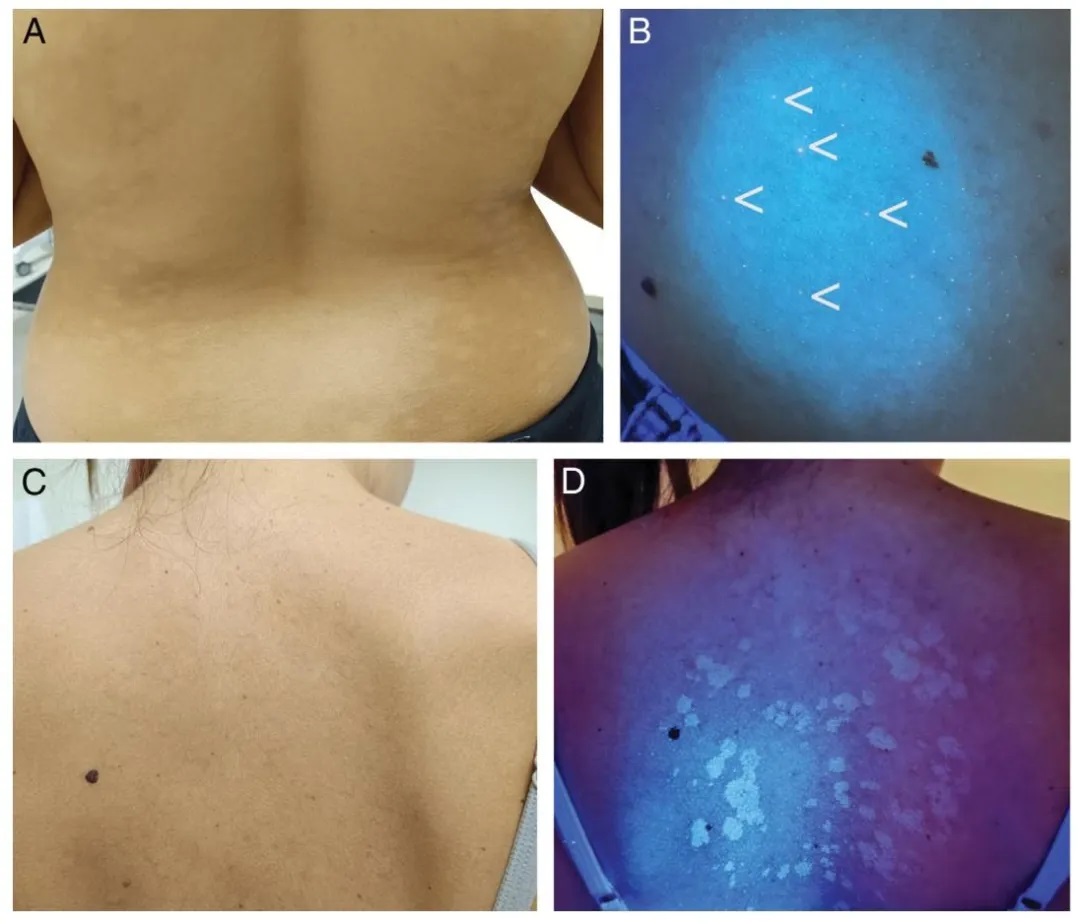
Figure 3.
(A) Progressive macular hypomelanosis.
(B) Under Wood’s lamp examination, red follicular fluorescence is observed in hypopigmented areas (more prominent to the naked eye than depicted in the image).
(C) Clinically subtle tinea versicolor.
(D) Yellow fluorescence under Wood’s lamp examination.
Progressive Macular Hypomelanosis (PMH)
Caused by Propionibacterium acnes, PMH presents with red follicular fluorescence due to coproporphyrin III accumulation. WL distinguishes PMH from tinea versicolor (yellow-green glow), pityriasis alba (no fluorescence), and idiopathic guttate hypomelanosis (bluish-white spots), improving diagnostic specificity.
Role in Infectious Dermatology
Erythrasma
A hallmark of Corynebacterium minutissimum, erythrasma shows a distinct coral-red fluorescence due to porphyrin production. This pattern helps differentiate it from non-fluorescent intertriginous dermatoses such as inverse psoriasis or candidiasis.
Dermatophyte Infections
WL helps identify specific fungal infections:
Tinea versicolor (Malassezia): Yellow-green fluorescence
Tinea capitis (Microsporum spp.): Blue-green hue
Favus (Trichophyton schoenleinii): Pale blue signal
Trichomycosis axillaris: White-yellow luminescence
Most Trichophyton species do not fluoresce
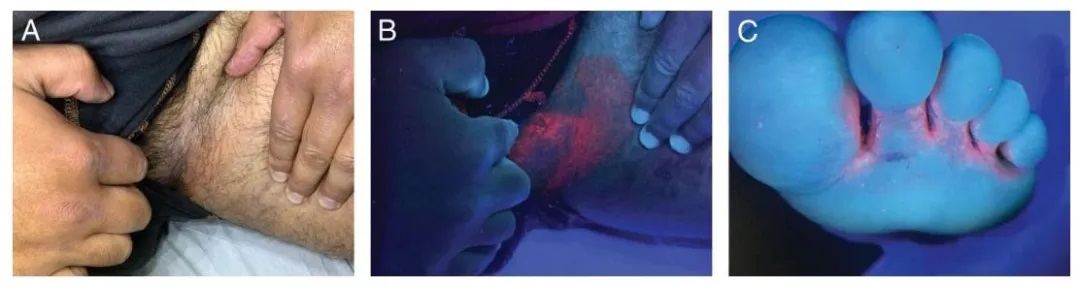
Figure 4.
(A) Erythrasma in the groin region.
(B) Coral-red fluorescence observed under Wood’s lamp examination.
(C) Erythrasma between the toes of the left foot, showing coral-red fluorescence under Wood’s lamp.
Pseudomonal Infections
Pseudomonas aeruginosa emits fluorescein, detectable as a vivid green glow under UV light. WL proves effective in identifying wound infections and green nail syndrome, allowing for prompt antimicrobial treatment.
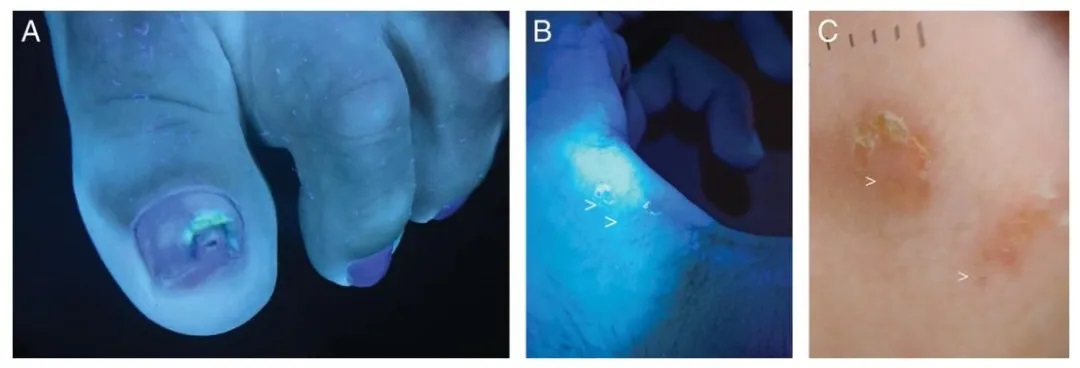
Figure 5.
(A) Green nail syndrome caused by Pseudomonas aeruginosa.
(B) Scabies burrow under Wood’s lamp (indicated by white arrow).
(C) Dermoscopic image of a scabies burrow (indicated by white arrow).
Use in Parasitic Dermatoses
Scabies
WL examination illuminates mite burrows as bluish-white linear tracks, with the mite body itself sometimes glowing white or green. UV365 dermoscopy further enhances mite visibility, aiding diagnosis in atypical cases.
Application in Cutaneous Oncology and Surgery
Lentigo Maligna
Delimiting LM margins is challenging due to subclinical extension. While current guidelines suggest 5–10 mm surgical margins, a large cohort study indicated that 15 mm may be required for a 97% complete excision rate.
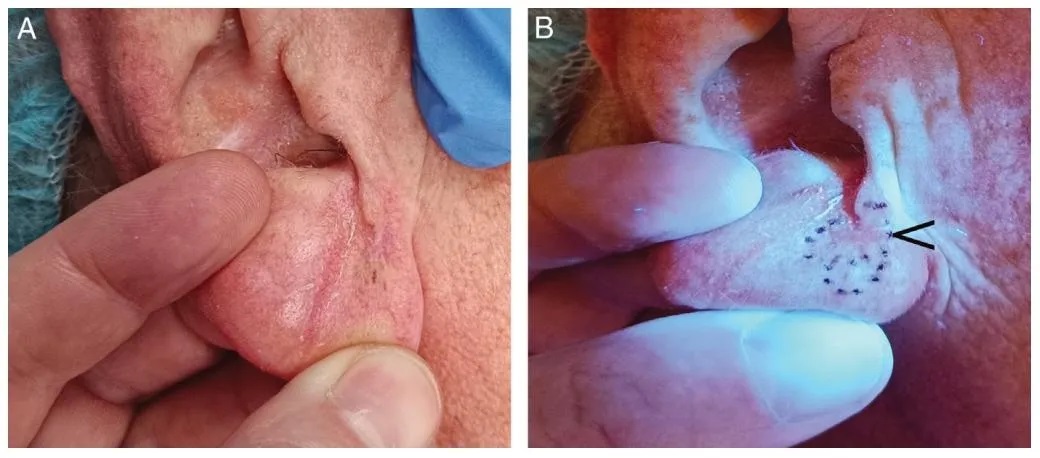
Figure 6.
(A) Malignant lentiginous nevus on the right earlobe, with poorly defined clinical margins.
(B) Enhanced margin delineation under Wood’s lamp, allowing for precise boundary identification during the first stage of Mohs micrographic surgery. The black arrow indicates the site of a previous biopsy, which is clearly visible under Wood’s lamp.
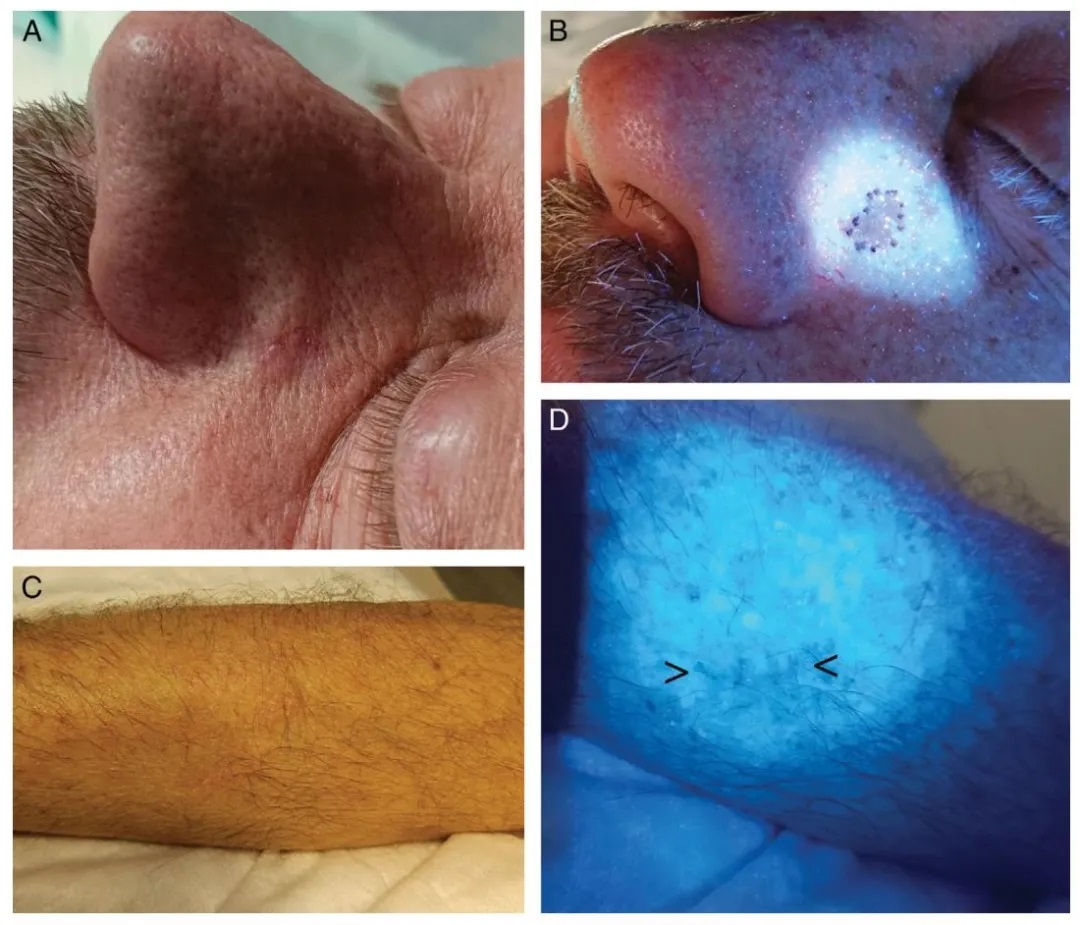
Figure 7.
(A) Basal cell carcinoma with indistinct margins on the left nasofacial fold.
(B) Preoperative margin demarcation using Wood’s lamp.
(C) Postoperative scar following excision of melanoma on the right forearm, with clinically unapparent extension prior to planned re-excision.
(D) Wood’s lamp easily highlights the scar (indicated by the black arrow).
Wood’s lamp accentuates melanin-rich tumor margins against surrounding fluorescent normal skin. Its preoperative use in Mohs surgery improves boundary assessment and may reduce recurrence. One prospective study demonstrated that WL-guided margin mapping aligned with final histological margins in 88% of cases when a 5 mm buffer was added beyond the clinically visible border.